Gynecomastia
Gynecomastia comes from the Greek meaning “gyne” meaning woman and “mastos” meaning breasts. It refers to abnormal development of large mammary glands in males. The diagnosis can be made by physical examination where relatively firm tissue (breast gland tissue) can be differentiated from relatively soft tissue (adipose tissue). Breast prominence due to excessive adipose tissue is called pseudo-gynecomastia or lipomastia. The differentiation of true gynecomastia from adipose tissue is important because the surgical treatment may differ. Usually physical examination by a well experienced board-certified plastic surgeon is sufficient to make the diagnosis and to determine the best course of treatment.
CONTACT US
About

Gynecomastia is defined as the visible or palpable development of breast tissue. Gynecomastia is a condition in which males develop enlargement of the breast and/or “puffy” areola. This is quite common in adolescents and is often first noted at the onset of puberty. Gynecomastia affects an estimated 40% to 60% of men. It may affect only one breast or both. When gynecomastia is severe, when it persists, and in those cases where there is suspicion of malignancy surgical treatment may be indicated.
For men who feel self-conscious about their appearance, breast-reduction surgery can help. The procedure removes fat and or glandular tissue from the breasts, and in extreme cases removes excess skin, resulting in a chest that is flatter, firmer, and better contoured. In most cases, the incisions for this operation can be placed just inside the areolar border where they are less likely to be conspicuous. Gynecomastia is often best treated with partial excision of the prominent glandular tissue as well as liposuction surgery of the peripheral chest area. If the prominence of the chest wall is caused by adipose tissue, then liposculpture surgery alone may suffice.
It is always best to be at a long term stable weight prior to surgery. Accurate diagnosis would necessitate physical examination. It is important to differentiate gynecomastia (excess breast tissue) from lipomastia ( otherwise known as pseudo-gynecomastia or excess adipose tissue of chest wall). Pubertal gynecomastia often resolves within 1 to 3 years after onset. Adult onset gynecomastia however does not necessarily do so. Breast glandular tissue “can go away” without surgical intervention; this is most commonly seen in pubertal gynecomastia. Once gynecomastia has been present for longer than a year, it is unlikely to spontaneously resolve.
Our Patients
Love Us!
Take a look at what some of our many happy patients say about their experience at Prime Plastic Surgery.
Candidates

Men who have abnormally large breasts, called gynecomastia, can also benefit from breast reduction surgery. This abnormal appearing chest contour can be improved with male breast reduction surgery. The results of the procedure are significant and permanent. The benefits of male breast reduction are not only physical – producing firmer, flatter, more masculine chest contours – but emotional as well as self-esteem is many times improved.
This corrective procedure, however, is not a replacement for diet and exercise for the patient who is significantly overweight. Our doctors use techniques to achieve a natural, masculine appearance. Most men who have undergone breast reduction report a boost in their self-esteem and confidence.
CONSULTATION PROCESS
During the consultation process, a history and physical examination will likely be very helpful. Make sure you provide a list of all medications and/or drugs you use. Hormonal studies, although sometimes helpful, are not mandatory.
Procedure
The glandular tissue must be removed. This firm fibrous tissue extends from the nipple areolar complex down to the surface of the pectoral muscle beneath. In some cases, it is helpful to use liposuction to remove some of the fatty tissue which always surrounds this ductal tissue. Without this liposuction some patients would have a “donut” shaped defect after removal of the ductal tissue.
Treatment will differ depending on diagnosis. In most cases, gynecomastia is treated with resection of the excess breast tissue; peripheral chest liposuction surgery may also be helpful.
The most common complication following surgical removal of the ductal tissue is hematoma. When severe this could lead to a second operation to drain the collection of blood. Some residual deformity of the nipple areolar area may remain despite the best efforts of the surgeon. As with any operation, a wound infection could occur. Inadvertent injury to the blood supply of the nipple areolar region could result in loss of skin in the nipple areolar area. There would be the usual anesthetic risks associated with any surgical procedure.
One other potential risk associated with gynecomastia surgery is contour deformity related to over resection of glandular tissue and/or adipose tissue. This is a risk that is explained to patients who are undergoing the procedure. Many patients who have gynecomastia are looking for the chest to be as flat as possible. Surgeons must balance their desire to achieve the patient’s goals with efforts to avoid over resection and contour deformity.These complications and other even rarer complications do not occur often and the vast majority of patients undergoing this operation are very pleased and adopt a more normal life style with regard to exposure of the chest in normal social situations such as the beach.
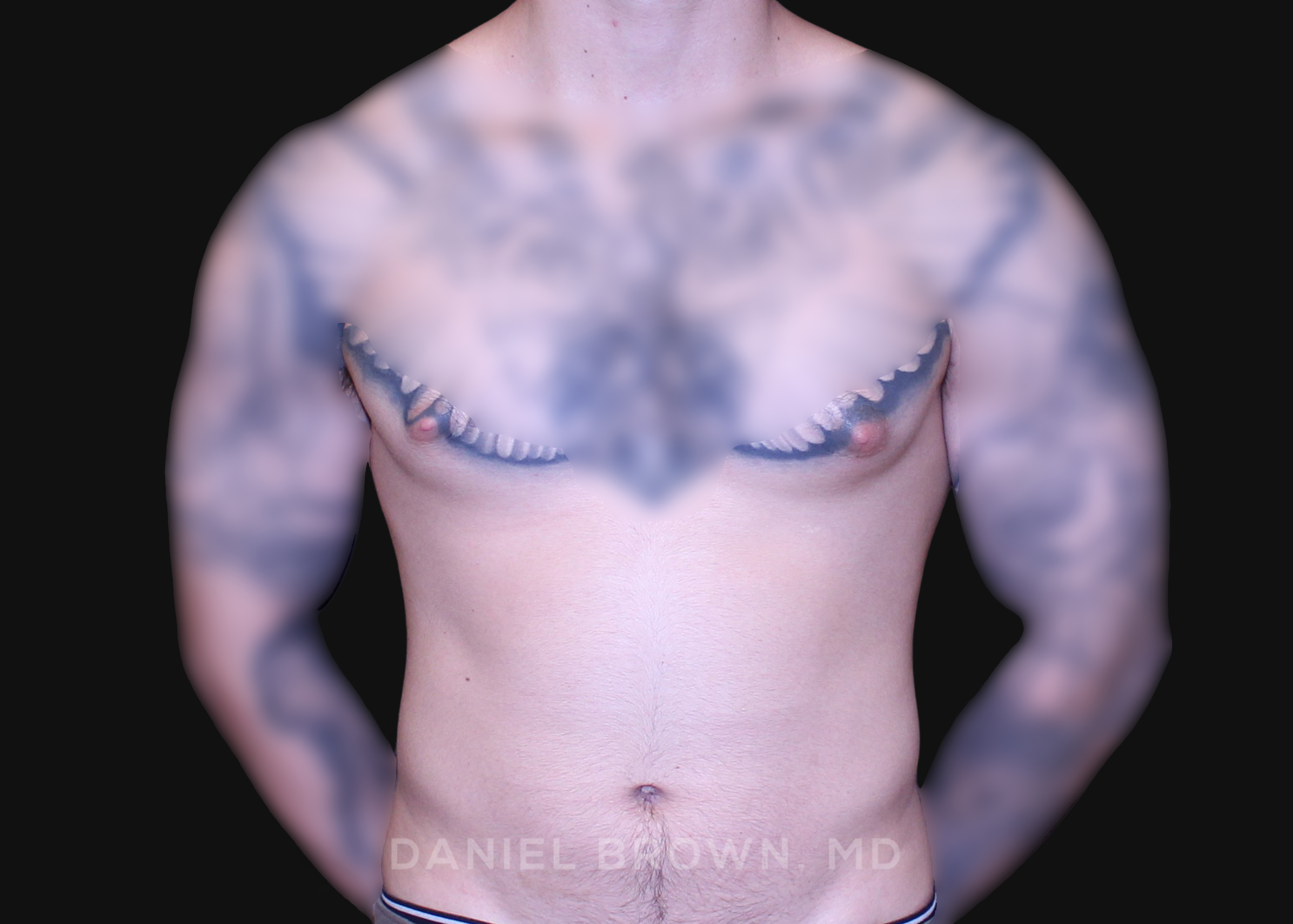
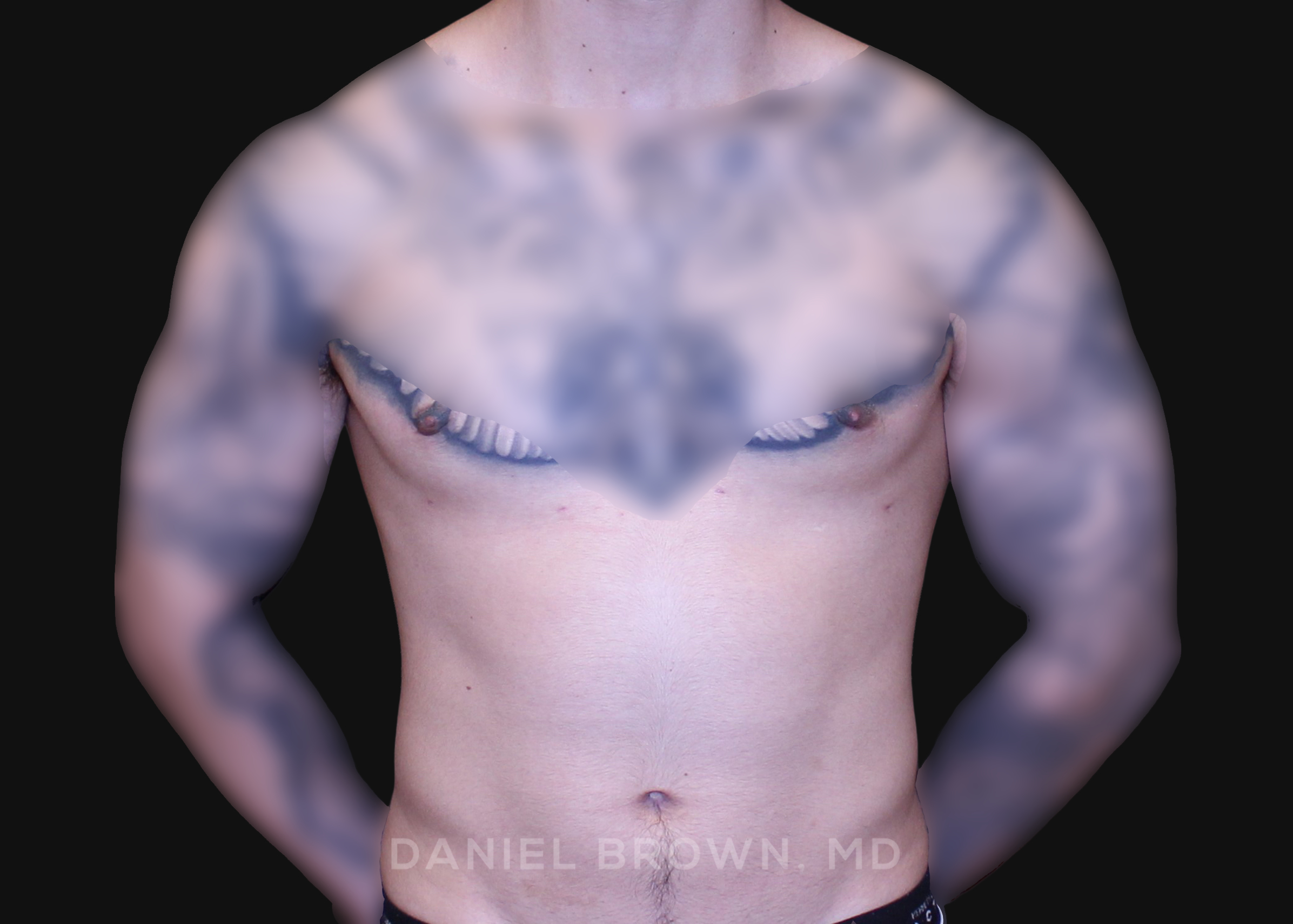
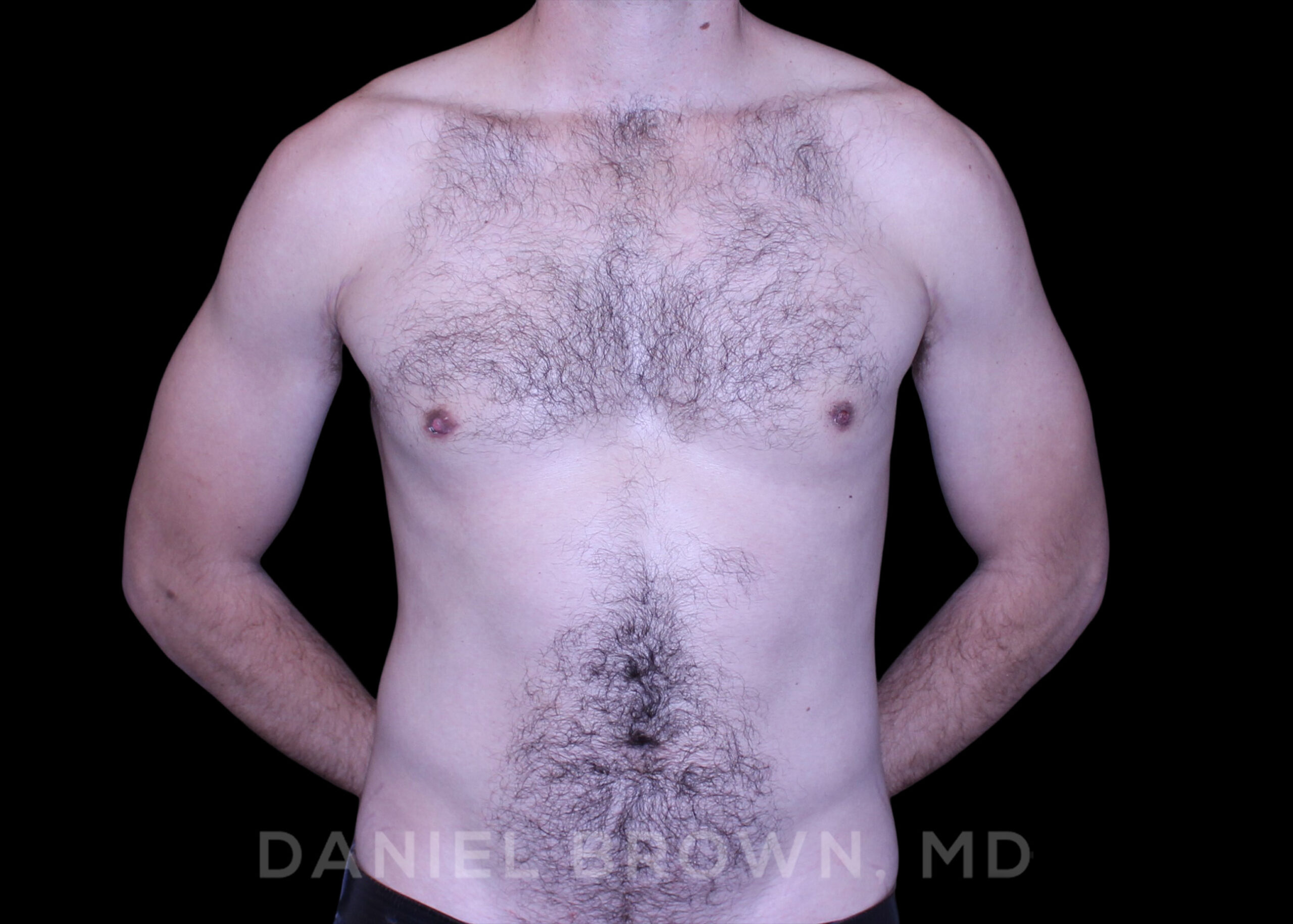
OUR BEFORE & AFTERS
The gallery contains before and after pictures of actual patients. View all cases for a complete listing of all our before and after photos of the patients treated.
RECOVERY
Mild swelling is to be expected after surgery, especially as you become more active. Compression garment will be worn for the first month after surgery. The degree of swelling that occurs after gynecomastia surgery will depend on the exact procedure performed. For example, swelling tends to be greater with larger areas treated, especially with liposuction surgery. Generally however, swelling tends be mild to moderate and well tolerated. Long-term you be able to return to all forms of exercises/activities after gynecomastia surgery.
Recovery after gynecomastia can vary for each patient depending on the severity and complexity of each case. Generally, patients are asked to avoid strenuous activity and heavy-lifting or about 4-6 weeks. This decreases risks of complications. However, patients can exercise within 2-4 weeks, focusing on other areas, like the lower extremities.
CONTACT US

Telephone No.619-466-8851